Death Spiral of Dysphagia
To Fight for Food and Life
by Dr Gabriël Roux
68% of aged care residents in Australia are either malnourished or at high risk of malnutrition1.
Dysphagia affects 50-60% of nursing home residents2
80% of dysphagia cases in older adults remain undiagnosed3
What a desperate state of affairs
My Fellow Colleagues, Service Providers and Carers in the Aged Care Industry.
We seem to have slipped into an air of nonchalance that has left us impatient with Dementia and intolerant to the tremors and incoherence of those at the final round on the rostrum.
This may be because we compare this stage to the earlier stages of life, thereby diminishing its significance and tarnishing its dignity.
Perhaps we are understaffed and overworked.
Perhaps we are overwhelmed by the rapid increase in the number of the elderly to care for.
Regardless of the underlying cause, the consequences are profoundly tragic.
In caring for the frail and those with dementia and dysphagia, we frequently fall short of delivering the essential minimum of 1,500 ml of fluids and 1,500 kcal of nutrition daily. We dutifully chart the weight loss, yet we overlook its direct link to the creeping horror of starvation, the silent killer that erodes dignity and eventually destroys life itself.
Why do we experience this persistent blind spot in connecting cause and effect?
It stems from a deeply ingrained mindset of detachment that is quite prevalent industry-wide. See the Story of Rose Palmada at the end.
We rationalise: If a person with dementia refuses food, it must be their unspoken desire to end life.
If feeding demands precious minutes we lack, we blame the overburdened system.
And if the elderly have reached this vulnerable stage of life, why extend life further?
This troubling pattern of thought and inaction is far from isolated to Australia; it echoes globally, requiring a reform of how we perceive and care for our senior citizens.
So, the Australian Royal Commission into Aged Care Quality and Safety (2018 to 2021) shocked us back into reality. The Commission expressed profound concern and dismay at the "shocking" and "unacceptable" state of aged care, describing the systemic neglect, including inadequate nutrition and lack of dignity, as a "national disgrace" that failed to respect the fundamental human rights of older Australians. Commissioners labelled the situation a "sad and shocking system that diminishes Australia," highlighting substandard care that left many elderly malnourished and dehumanised.
Is this a new phenomenon? No.
Jonathan Swift’s Gulliver’s Travels (1726) portrays the Struldbrugs, decaying elderly, as “despised and hated”. William Shakespeare’s King Lear (1605) captures the vulnerability of old age when Lear cries, “I am old and foolish,” abandoned by those meant to care for him. And Leo Tolstoy in The Death of Ivan Ilyich (1886) echoes his cry: “I am becoming a burden”.
But when we see wrong and infelicitous, we can be sure that correct, appropriate and felicitous exist as well.
In Cicero’s famous essay On Old Age (De Senectute), written in 44 BC, Cicero wrote: “The old man, if he has lived well, is honoured and loved; his age is not a burden but a crown of dignity.”
Pearl S. Buck said, “Our society must make it right and possible for old people not to fear the young or be deserted by them, for the test of a civilisation is the way that it cares for its helpless members.”

So, what does the
problem look like?
A 2017 national study of 60 residential aged care services found that 68% of residents were malnourished or at high risk of malnutrition.
Witness Testimonies: In the inaugural Adelaide hearing (February 2019), family members Barbara Spriggs and Clive Spriggs testified about their relative Bob's severe dehydration and undernourishment at an Adelaide facility, where he was admitted twice and suffered rapid health decline, including unexplained bruising and medication errors. They described how neglect led to his inability to access fluids, contributing to his overall mistreatment. Similar accounts from over 600 witnesses highlighted dehydration as a "silent killer," with elderly residents denied timely hydration due to rushed care and insufficient assistance.
Expert and Systemic Evidence: A 2017 national nutrition study cited in the final report (Care, Dignity and Respect, Volume 2) revealed that up to 68% of residents were malnourished or at high risk, with dehydration frequently intertwined—evidenced by low fluid intake (often below the 1,500 ml daily minimum) and inadequate screening tools. Dietitians and clinicians submitted data showing dehydration's links to pressure injuries and delirium, exacerbated by dysphagia in dementia patients, where thickened fluids were inconsistently provided.
The Royal Commission concluded on malnutrition and dehydration: Poor nutrition directly contributed to serious outcomes, including falls, fractures, pressure injuries, infections, and unnecessary hospitalisations. Dehydration was a related concern, exacerbated by inadequate monitoring and support for swallowing difficulties (dysphagia).
So, what happens if we miss the diagnosis of Dysphagia or the malnutrition and dehydration that follow from it? What happens if we make the diagnosis but then fail to care sufficiently?
The patient/client gets caught up in the Death Spiral of Dysphagia.
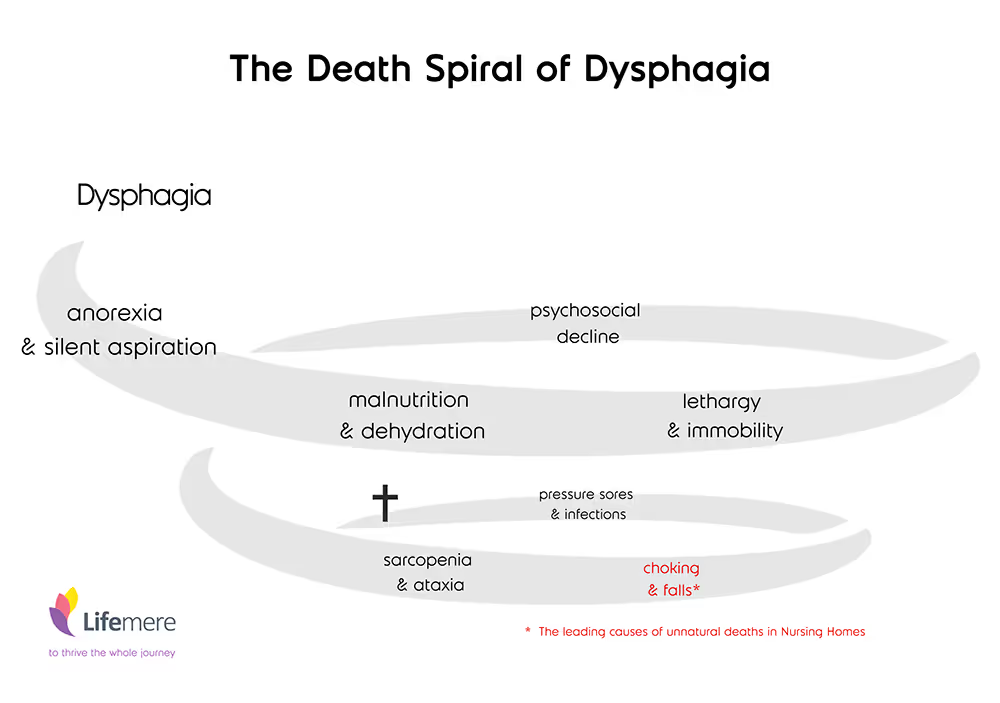
Dysphagia unchecked would typically initiate a Spiral of Death.
This cascade of events is interlinked. Dysphagia often begins quietly, with symptoms like loss of appetite and difficulty swallowing, sometimes accompanied by silent aspiration, where food enters the airways unnoticed. This creates a risk of inadequate intake, inadvertently sliding residents into a state of malnutrition and dehydration. As a result, they become lethargic, sleeping through much of the day, and become increasingly confined to chairs or beds, setting the stage for a devastating decline.
A marked psychosocial deterioration follows, where laughter and enjoyment dissipate, speech becomes less and social interaction all but disappears. Inactivity and malnutrition lead to sarcopenia (loss of muscle bulk) and ataxia (poor balance and unstable gait). At this stage, the dysphagia often has deteriorated beyond subclinical aspiration. Overt choking that could be life-threatening now becomes a significant risk. This stage could pose terrifying experiences for the patient, who not only fears death due to asphyxia but may experience excruciating episodes when inhaling food into the airways. The tragic reality at this stage is that the patient is often dysphasic (unable to communicate their distress) due to the stage of deterioration and can only express his fear by rejecting food and liquids. The second risk at this stage is falls with head injuries and fractures due to the poor state of muscle, tendon and reflex (proprioceptive) function. This stage carries a significant mortality. According to Ibrahim et al, the most common cause of unnatural deaths in residential aged care facilities is falls, followed by choking. If the patient survives this stage and has not already suffered from bladder and chest infections, this will most likely now follow in the wake of an inability to walk (permanently bedridden), contractures, bedsores and often septicaemia. We usually intervene at this stage to hasten the inevitable by implementing palliative care measures.
Sadly, we miss the diagnosis of Dysphagia in 83,000 nursing home residents in Australia per year. And even if we do get the diagnosis right, we regularly fail in our duty of care.

How is it possible to regularly
miss the diagnosis of
malnutrition and dehydration?
Dehydration in the elderly skin and malnutrition in the frail could pose a diagnostic difficulty. The loss of turgor (firmness) in the skin can be masked by age-related atrophic changes and go unnoticed due to poorly recorded or inaccurate fluid balance charts. Subtle emaciation might go unnoticed and unreported due to poor weight recordings.
So, we commonly concentrate on the prevailing problem of bladder or lung infections, falls or pressure sores. In the process, we overlook the underlying cause: Dysphagia and the subsequent malnutrition and dehydration that follow. This diagnosis missed would likely result in the tragic cascade of the “Death Spiral” leading to often literally unspoken suffering, distress, loss of dignity, despair of family and friends, the premature implementation of palliative care measures, and finally a premature and quite frankly, an iatrogenic death.
How do we prevent this tragic pathway?
Royal Commission Findings and Recommendations:
The report (Volume 3A) recommends mandatory hydration screening using validated aged care tools, workforce training for fluid balance monitoring, and enforceable standards (e.g., Standard 5 on clinical care) to prevent it. Post-report reforms, including the 2024 Aged Care Act, mandate early detection processes, reflecting the urgency of the evidence.
The early diagnosis and correct management of Dysphagia:
- If a patient loses ≥5% body weight in 1 month or ≥7.5% in 3 months, implement daily weight recordings5, calorie intake charts (target ≥1,500 kcal/day)6, and fluid balance charts (target ≥1,500 ml/day)7, with oversight by trained staff to ensure accuracy8.
- 1–2 weeks, screen for dysphagia (e.g., EAT-10, speech pathology assessment)9.
- Presume dysphagia-related dehydration and malnutrition until proven otherwise10, and initiate interventions like texture-modified food, thickened liquids11, and specialised feeding devices.
The Royal Commission's 148 recommendations for a reformed aged care included workforce upskilling (e.g., training on IDDSI), multidisciplinary care (including early input by a Speech Pathologist) and activity-based funding to ensure equitable access.
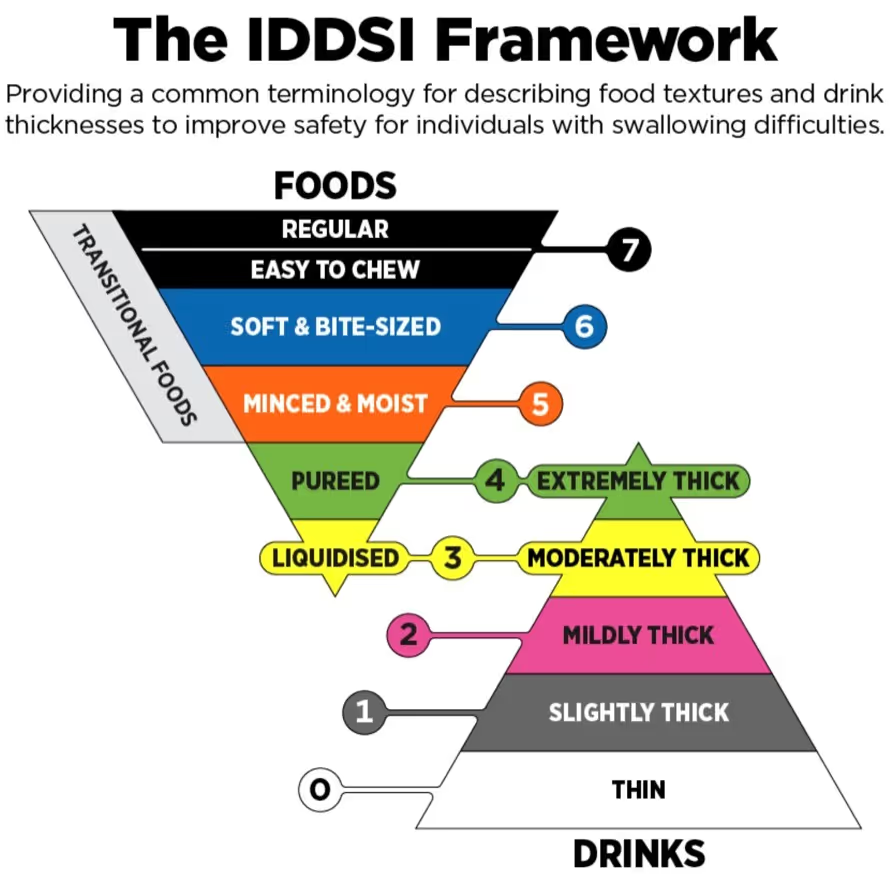
Thickened Liquids
- Prescribe thickened liquids (e.g., IDDSI Levels 1–4) based on speech pathology recommendations to control flow rates and enhance swallow safety, targeting a minimum fluid intake of 1.5L/day to combat dehydration.
- Integrated into broader nutrition guidelines under Recommendations 19 and 38, with staff training required to prepare and administer thickened fluids accurately, ensuring compliance with clinical standards and resident preferences.

Texture-Modified Foods
- Adopt standardised texture modifications (e.g., per the International Dysphagia Diet Standardisation Initiative, IDDSI framework) to ensure foods are safe, palatable, and nutritionally adequate, reducing choking and aspiration risks.
- Recommendation 19 urges an urgent review of Aged Care Quality Standards to incorporate best-practice nutrition support, emphasising desirable, culturally appropriate meals with texture adjustments tailored to individual needs, overseen by dietitians and speech pathologists.

Assistive Cups/Utensils and Safeguarding Liquid Intake
- Recommendation 36 mandates improved access to allied health services (e.g., occupational therapy) to facilitate safe, dignified oral intake with “adaptive equipment” (Volume 1, p. 76)
- Recommendation 38 reinforces funding for allied health in residential care, enabling the provision of utensils that minimise spillage and promote independence, alongside training for care staff on safe feeding techniques.

Conclusions:
Who do we blame?
The doctor who missed the diagnosis, the staff who recorded the weight and fluid balance charts, poor management at the facility, insufficient guidelines and funding by the government?
Read the story of Rose Palmada and her family to understand the mindset that we are trying to address: The Story of Rose
I think, wherever I come from, I need to clean my house.
We need to change our mindset and our demeanour
towards the seniors in our society.
We need to restore respect and appreciation
for their new reality on their terms.
We need to uphold dignity.
We need to love and feed and venerate life
until its natural consequence.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript
An estimated 80% of cases are un-diagnosed. Early diagnosis allows for rehabilitation before complications make rehabilitation increasingly difficult.
General signs may include:
- Coughing during or right after eating or drinking
- Wet or gurgly sounding voice during or after eating or drinking
- Extra effort or time needed to chew or swallow
- Food or liquid leaking from the mouth or getting stuck in the mouth
- Recurring pneumonia or chest congestion after eating
- Weight loss or dehydration from not being able to eat enough
Complications:
- Poor nutrition or dehydration with weight loss
- Risk of aspiration which can lead to pneumonia and chronic lung disease
- Less enjoyment or even fear of eating or drinking
- Embarrassment or isolation in situations involving eating
The causes of swallowing disorders in:
.avif)
Adults
Damage to the nervous system, such as:
- Amyotrophic Lateral Sclerosis
- Muscular Dystrophy
- Cerebral Palsy
- Alzheimer's Disease
- Stroke
- Brain Injury
- Spinal cord injury
- Parkinson's Disease
- Multiple Sclerosis
- Dementia
.avif)
Infants & Children
- Cleft lip/palate
- Developmental Disability
- The RoseCup system is not currently suitable for use in babies
Problems affecting the head& neck, including:
- Cancer in the mouth, throat or esophagus
- Injury or surgery involving the head and neck
- Decayed or missing teeth, or poorly fitting dentures
Early diagnosis
An estimated 75% of cases are un-diagnosed. Early diagnosis allows for rehabilitation before complications make rehabilitation increasingly difficult.
Speech Pathologists have a pivotal role in the assessment and management of Dysphagia.
It is recommended that any person who knows or suspect they have a swallowing disorder should contact a local Speech Pathologist that specialise in Dysphagia, to assist them to evaluate their swallowing and perform special tests necessary for assessments and screenings.
























-- / 5 average rating from -- reviews
We'd love to hear your thoughts!
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.
We'd love to hear your thoughts!
-- / 5 average rating from -- reviews
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere. uis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae era